Understanding Yeast Infection Medicine: Causes, Treatments, and Prevention
Yeast infections, also known as candidiasis, are a common health issue that affects millions of people worldwide, particularly women. If you’re searching for information on yeast infection medicine, you’re likely looking for reliable ways to address this uncomfortable condition. This comprehensive guide explores the basics of yeast infections, their symptoms, available treatments, and preventive measures. Remember, while this article provides general information, it’s essential to consult a healthcare professional for personalized advice. Self-diagnosis or treatment without medical guidance can lead to complications.
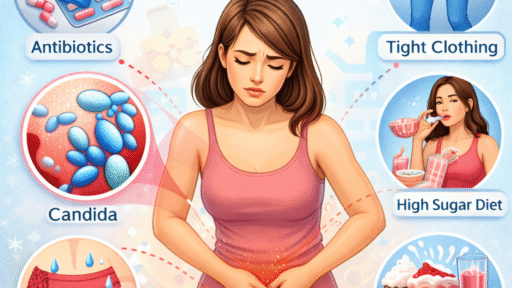
What Is a Yeast Infection?
A yeast infection occurs when there’s an overgrowth of Candida, a type of fungus naturally present in the body. Candida albicans is the most common culprit, thriving in warm, moist areas like the vagina, mouth, or skin folds. Vaginal yeast infections are the most prevalent, affecting about 75% of women at some point in their lives, according to health organizations like the Centers for Disease Control and Prevention (CDC).
Factors that can trigger this overgrowth include antibiotics, which disrupt the body’s bacterial balance; hormonal changes during pregnancy or menopause; uncontrolled diabetes; weakened immune systems; and even lifestyle habits like wearing tight clothing or using scented hygiene products. Understanding these triggers is key to choosing the right yeast infection medicine and preventing recurrences.
Common Symptoms of Yeast Infections
Recognizing the signs early can help you seek appropriate yeast infection medicine sooner. For vaginal yeast infections, symptoms often include:
- Intense itching and irritation in the vaginal area
- Thick, white, cottage cheese-like discharge
- Burning sensation during urination or intercourse
- Redness and swelling of the vulva
In men, yeast infections (balanitis) might cause redness, itching, or a rash on the penis. Oral thrush, another form, presents as white patches in the mouth, soreness, and difficulty swallowing. Skin-based yeast infections can appear as red, itchy rashes in areas like the armpits or groin.
If symptoms persist or worsen, it’s crucial to see a doctor, as they could indicate a more serious condition like bacterial vaginosis or a sexually transmitted infection (STI). Misdiagnosing can delay effective treatment.
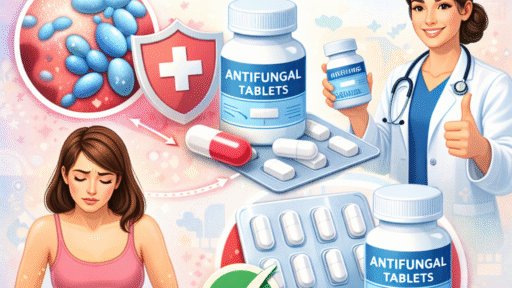
Types of Yeast Infection Medicine
When it comes to yeast infection medicine, options range from over-the-counter (OTC) remedies to prescription treatments. The choice depends on the infection’s severity, location, and frequency.
Over-the-Counter Yeast Infection Medicine
Many yeast infections can be treated with OTC antifungal medications, which are widely available at pharmacies. These typically contain active ingredients like miconazole, clotrimazole, or tioconazole. Popular forms include:
- Creams and Suppositories: Products like Monistat (miconazole) or Gyne-Lotrimin (clotrimazole) are inserted vaginally for 1 to 7 days. A single-dose option like Monistat 1 provides convenience for mild cases.
- Oral Tablets: Fluconazole (available as Diflucan in prescription form, but some OTC versions exist in certain regions) is taken as a pill for systemic relief.
- Ointments for Skin Infections: For external or skin-based issues, creams like Lotrimin AF work by targeting the fungus directly.
These OTC yeast infection medicines are effective for about 80-90% of uncomplicated cases, as per studies from the American College of Obstetricians and Gynecologists (ACOG). Always follow the package instructions and complete the full course to avoid resistance.
Prescription Yeast Infection Medicine
For recurrent or severe infections, a doctor may prescribe stronger yeast infection medicine. Common prescriptions include:
- Fluconazole: A single oral dose or weekly maintenance for chronic cases.
- Terconazole or Butoconazole: Vaginal creams or suppositories for resistant strains.
- Boric Acid Suppositories: Used under medical supervision for non-albicans Candida species, though not FDA-approved for this purpose.
- Nystatin: Often for oral thrush, available as a liquid or lozenge.
If the infection is linked to underlying conditions like diabetes or HIV, addressing those is part of the treatment plan. Prescription options ensure tailored yeast infection medicine, reducing the risk of side effects.
Natural and Home Remedies as Complementary Approaches
While not substitutes for medical yeast infection medicine, some natural remedies can support treatment. Probiotics, found in yogurt or supplements, may help restore bacterial balance. Tea tree oil or coconut oil have antifungal properties in lab studies, but they should be diluted and used cautiously to avoid irritation.
Garlic, with its allicin compound, is sometimes touted as a natural antifungal, but evidence is anecdotal. Always discuss these with a healthcare provider, as they might interact with prescribed yeast infection medicine.
How Yeast Infection Medicine Works
Antifungal yeast infection medicines target the cell walls of Candida, disrupting their growth. Azoles (like miconazole) inhibit ergosterol production, a key fungal component, while polyenes (like nystatin) bind to the cell membrane, causing leakage.
For best results, apply treatments at bedtime to minimize leakage. Side effects are rare but can include mild burning or allergic reactions. If you’re pregnant, only use recommended yeast infection medicine, as some OTC options aren’t safe.
Diagnosing Yeast Infections Before Treatment
Before starting any yeast infection medicine, accurate diagnosis is vital. A pelvic exam or microscopic analysis of discharge can confirm Candida. Home test kits measure vaginal pH but aren’t foolproof. Recurrent infections (four or more per year) warrant further tests for underlying issues.
Prevention Strategies to Reduce Reliance on Yeast Infection Medicine
Preventing yeast infections can minimize the need for medicine. Key tips include:
- Wear breathable cotton underwear and avoid douching.
- Maintain good hygiene without over-washing, as it disrupts natural flora.
- Control blood sugar if diabetic.
- Use condoms during sex if infections recur.
- Incorporate probiotic-rich foods like kefir or sauerkraut.
Lifestyle changes, combined with prompt treatment, can keep infections at bay.
Yeast Infections in Special Populations
Yeast Infections During Pregnancy
Hormonal shifts make pregnant women more susceptible. Safe yeast infection medicine includes 7-day topical azoles; avoid oral fluconazole in the first trimester due to potential risks.
Yeast Infections in Men and Children
Men might need topical creams, while children’s oral thrush often resolves with nystatin. Always seek pediatric advice.
Chronic or Recurrent Yeast Infections
For those with frequent episodes, long-term suppressive therapy with weekly fluconazole may be prescribed. Identifying triggers like diet or stress is crucial.
Myths and Misconceptions About Yeast Infection Medicine
Common myths include yeast infections being solely STIs (they’re not) or that sugar causes them directly (it contributes but isn’t the sole factor). Another is that all discharge indicates infection—normal variations exist. Reliable information debunks these, ensuring informed choices.
When to Seek Professional Help
If OTC yeast infection medicine doesn’t resolve symptoms in 3-7 days, or if you experience fever, abdominal pain, or foul-smelling discharge, see a doctor immediately. Untreated infections can spread, leading to complications like pelvic inflammatory disease.
The Role of Diet and Lifestyle in Managing Yeast Infections
A low-sugar, anti-inflammatory diet may help prevent overgrowth. Foods like garlic, onions, and cruciferous vegetables support gut health. Exercise and stress management bolster immunity, reducing infection risk.
Emerging Research on Yeast Infection Treatments
Recent studies explore probiotics like Lactobacillus strains for prevention. Antifungal resistance is a concern, prompting research into new compounds. Stay updated via reputable sources like PubMed.
Conclusion
Yeast infection medicine offers effective relief for this common ailment, from OTC creams to prescription options. By understanding causes, symptoms, and prevention, you can manage and reduce occurrences. Always prioritize professional medical advice over self-treatment. This knowledge empowers better health decisions



Understanding Yeast Infection Medicine: Causes, Treatments, and Prevention” is well-written, comprehensive, and informative. It demonstrates strong health communication skills and effectively balances medical accuracy with reader-friendly language.