Understanding Type 2 Diabetes: Causes, Symptoms, Risk Factors & Prevention
Type 2 diabetes is one of the most common long-term health conditions worldwide. It affects millions of people every year and continues to grow in both developed and developing countries. While only a healthcare professional can diagnose or manage diabetes, having a clear understanding of what Type 2 diabetes is—and recognizing the signs that may indicate risk—can help people make informed decisions about their health and lifestyle.
This article offers a comprehensive, educational, and AdSense-compliant overview of Type 2 diabetes, including symptoms, causes, risk factors, prevention tips, and when to consult a medical professional. It does not provide diagnosis, treatment instructions, or medical claims, and its sole purpose is to inform.
What Is Type 2 Diabetes?
Type 2 diabetes is a chronic metabolic condition that affects how the body regulates blood sugar (glucose). Under normal circumstances, the hormone insulin helps glucose move into cells, where it’s used for energy.
In Type 2 diabetes:
-
the body does not respond well to insulin (insulin resistance),
-
and/or the pancreas cannot make enough insulin to maintain normal blood sugar levels.
This results in higher-than-normal glucose in the bloodstream, which, over time, may lead to health complications if not properly managed by a professional.
How Type 2 Diabetes Develops
Type 2 diabetes usually develops gradually. Many people may not notice changes at first because symptoms can be mild or easily mistaken for everyday discomfort.
The development is usually linked to:
-
genetics
-
lifestyle habits
-
age-related changes
-
metabolic health
-
hormonal factors
Regardless of the cause, early detection allows people to seek timely medical evaluation and support long-term well-being.
Causes & Contributing Factors
There is no single cause of Type 2 diabetes. Instead, multiple factors increase likelihood. These include:
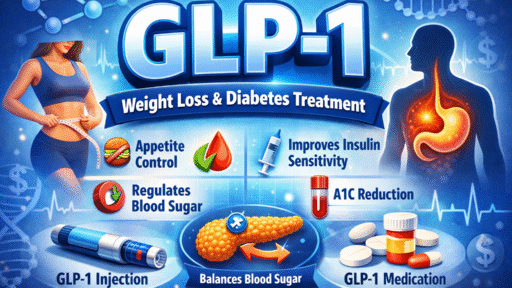
1. Insulin Resistance
This occurs when cells in muscles, fat, and the liver do not use insulin efficiently, causing glucose to build up in the bloodstream.
2. Genetics
Individuals with a family history of diabetes may have a higher risk, although genes alone do not determine the outcome.
3. Lifestyle Factors
While not always the cause, the following may influence risk levels:
-
limited physical activity
-
dietary patterns high in certain processed foods
-
long-term unhealthy weight patterns
4. Hormonal and Metabolic Factors
Hormonal changes and metabolic imbalances may affect how the body processes glucose.
5. Age
Although Type 2 diabetes can occur at any age, it becomes more common after the age of 40.
Common Symptoms of Type 2 Diabetes
Symptoms may develop slowly and vary from person to person. Not everyone will experience every symptom, and some people may have no noticeable signs at all, which is why regular medical checkups are important.
Common symptoms include:
-
increased thirst
-
frequent urination
-
unexplained hunger
-
fatigue and low energy
-
blurred vision
-
slow-healing wounds
-
skin dryness
-
frequent infections
-
tingling or numbness in hands or feet
These symptoms can also be related to other health conditions, which is why only a healthcare professional can offer accurate evaluation.
Why Early Recognition Matters
Recognizing symptoms early gives people a chance to consult a healthcare provider before complications develop. Professionals may use blood tests to assess glucose levels and offer guidance tailored to the individual’s needs.
Risk Factors for Type 2 Diabetes
Although anyone can develop Type 2 diabetes, some factors increase risk:
1. Family History
Having a parent or sibling with diabetes increases the likelihood.
2. Weight and Activity Patterns
Patterns of low activity or long-term unhealthy weight may contribute to insulin resistance.
3. Age
People over 40 are more likely to develop Type 2 diabetes.
4. Ethnicity
Some ethnic groups may have higher predisposition due to genetic and metabolic factors.
5. History of Gestational Diabetes
Women who develop diabetes during pregnancy may have an increased risk later in life.
6. High Blood Pressure or Cholesterol
These conditions may be linked to metabolic changes that affect glucose processing.
Again, these factors only suggest potential risk, not certainty.
How Type 2 Diabetes Is Diagnosed (General Overview)

Only a licensed healthcare provider can diagnose diabetes.
They may use tests such as:
-
Fasting blood sugar test
-
A1C test
-
Oral glucose tolerance test
These tests measure blood sugar levels over time and help professionals understand how the body is managing glucose.
Prevention & Risk-Reduction Tips
While not all cases can be prevented, certain lifestyle habits may support better metabolic health and reduce risk. These include:
1. Balanced Eating Patterns
Choosing a balanced, nutrient-rich eating plan may support healthier glucose levels.
2. Regular Physical Activity
Daily movement helps the body use glucose more efficiently.
3. Maintaining a Healthy Weight Pattern
Even modest weight changes may improve insulin response.
4. Reducing Stress
Stress affects hormone levels, which may influence glucose regulation.
5. Adequate Sleep
Healthy sleep patterns support proper metabolic function.
6. Routine Health Screenings
Regular checkups help identify early signs or risk factors before they become more serious.
These are general wellness practices, not medical treatment or cure. People with symptoms or risks should consult a healthcare provider.
Living With Type 2 Diabetes
Many individuals live full and healthy lives with Type 2 diabetes through:
-
professional medical guidance
-
lifestyle adjustments
-
regular monitoring
-
healthy routines
Healthcare providers may create personalized plans based on the individual’s needs and health status.
When to See a Healthcare Professional
It is advisable to speak with a professional if you notice these Symptoms Of Diabetes
-
multiple symptoms of high blood sugar
-
sudden changes in weight
-
increased thirst or urination
-
strong family history of diabetes
-
blurred vision
-
unusual fatigue
A medical professional is the only one who can provide diagnosis and appropriate guidance.