Understanding Endocrinologists: Specialists in Hormonal Health
In the complex world of modern medicine, specialists play a crucial role in addressing specific health concerns. One such specialist is the endocrinologist, a physician dedicated to diagnosing and treating disorders related to the endocrine system. If you’ve ever wondered, “What is an endocrinologist?” or “When should I see an endocrinologist?”, this comprehensive guide will provide in-depth insights. We’ll explore their roles, the conditions they manage, and why their expertise is vital for maintaining hormonal balance and overall well-being.
The endocrine system is a network of glands that produce hormones, which act as chemical messengers regulating various bodily functions. From metabolism and growth to reproduction and mood, hormones influence nearly every aspect of our health. When this system malfunctions, it can lead to a range of issues, making the endocrinologist’s role indispensable. In this article, we’ll delve into the intricacies of endocrinology, helping you understand how these specialists contribute to healthcare.
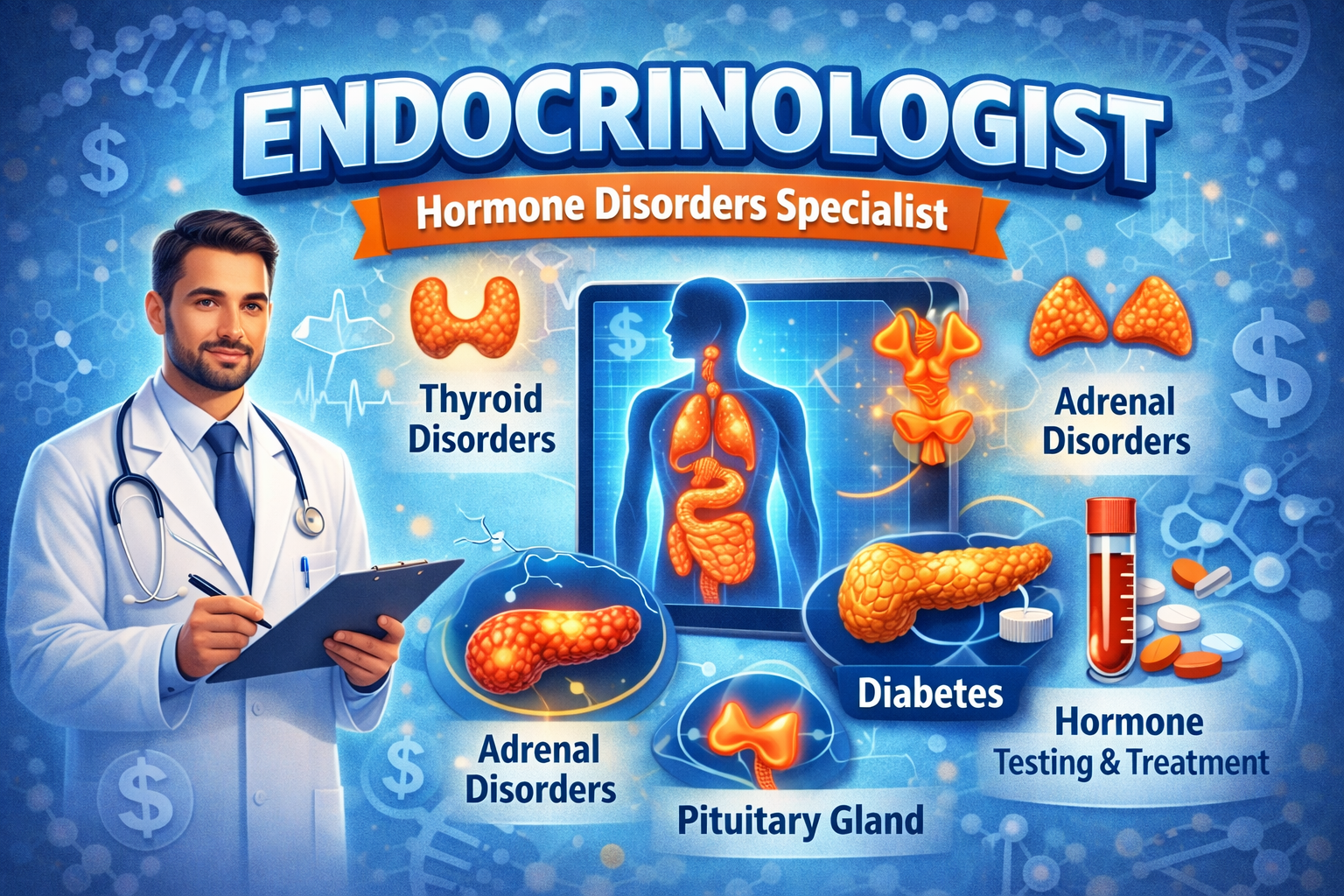
What Does an Endocrinologist Do?
An endocrinologist is a medical doctor who specializes in endocrinology, the branch of medicine focused on hormone-related diseases. After completing medical school, they undergo additional training in internal medicine followed by a fellowship in endocrinology, typically lasting 2-3 years. This rigorous education equips them to handle complex hormonal imbalances.
Their primary responsibilities include:
- Diagnosing Hormonal Disorders: Endocrinologists use advanced diagnostic tools, such as blood tests, imaging scans, and biopsies, to identify issues like thyroid dysfunction or adrenal gland problems.
- Developing Treatment Plans: They create personalized strategies, which may involve medications, lifestyle changes, or hormone replacement therapy. For instance, in cases of diabetes, they might prescribe insulin or oral medications while monitoring blood sugar levels.
- Managing Chronic Conditions: Many endocrine disorders are lifelong, requiring ongoing care. Endocrinologists work with patients to adjust treatments over time, preventing complications like heart disease or osteoporosis.
- Collaborating with Other Specialists: They often team up with primary care physicians, surgeons, or nutritionists for holistic care. For example, in treating polycystic ovary syndrome (PCOS), they might coordinate with gynecologists.
Endocrinologists also conduct research and educate patients on self-management techniques, such as diet modifications for metabolic disorders. Their expertise extends to pediatric endocrinology for children with growth issues or adult endocrinology for age-related hormonal changes.
Common Conditions Treated by Endocrinologists
Endocrinologists address a wide array of conditions stemming from glandular dysfunctions. Here are some of the most prevalent ones:
Diabetes Mellitus
Diabetes is one of the most common reasons people seek an endocrinologist. Type 1 diabetes occurs when the pancreas fails to produce insulin, while Type 2 involves insulin resistance. Gestational diabetes affects pregnant women. Symptoms include frequent urination, unexplained weight loss, and fatigue.
Treatment often includes:
- Blood glucose monitoring devices.
- Insulin therapy or medications like metformin.
- Dietary counseling to manage carbohydrate intake.
With rising global diabetes rates, endocrinologists are at the forefront of prevention through education on risk factors like obesity and family history.
Thyroid Disorders
The thyroid gland regulates metabolism via hormones like thyroxine (T4) and triiodothyronine (T3). Conditions include:
- Hypothyroidism: Underactive thyroid, leading to weight gain, depression, and cold intolerance. Treated with synthetic hormones like levothyroxine.
- Hyperthyroidism: Overactive thyroid, causing weight loss, anxiety, and rapid heartbeat. Management may involve antithyroid drugs or radioactive iodine.
- Thyroid Nodules and Cancer: Endocrinologists perform ultrasounds and fine-needle aspirations to detect malignancies.
Regular thyroid function tests are essential for early detection, especially in women over 50 who are more prone to these issues.
Adrenal Gland Disorders
The adrenal glands produce cortisol and aldosterone, crucial for stress response and blood pressure. Disorders like Addison’s disease (insufficient cortisol) or Cushing’s syndrome (excess cortisol) can cause fatigue, hypertension, or muscle weakness. Endocrinologists use ACTH stimulation tests for diagnosis and prescribe steroid replacements or surgical interventions.
Reproductive Endocrinology
Hormonal imbalances affect fertility and sexual health. Conditions include:
- Polycystic Ovary Syndrome (PCOS): Involves irregular periods, acne, and insulin resistance. Treatments range from birth control pills to fertility drugs like clomiphene.
- Menopause and Andropause: Endocrinologists manage symptoms like hot flashes or low testosterone with hormone replacement therapy (HRT), weighing benefits against risks like cardiovascular effects.
- Infertility: They investigate causes like low sperm count or ovulatory disorders, often recommending assisted reproductive technologies.
Bone and Calcium Disorders
Endocrinologists treat osteoporosis, where bones become brittle due to hormonal imbalances, often linked to parathyroid issues. Hyperparathyroidism leads to high calcium levels, causing kidney stones. Treatments include bisphosphonates or parathyroid surgery.
Pituitary Gland Disorders
The pituitary, known as the “master gland,” controls other endocrine glands. Tumors or deficiencies can lead to acromegaly (excess growth hormone) or hypopituitarism. MRI scans aid diagnosis, with treatments like dopamine agonists for prolactinomas.
These conditions highlight the endocrinologist’s broad scope, addressing everything from metabolic syndromes to rare genetic disorders like multiple endocrine neoplasia.
When Should You See an Endocrinologist?
Not every hormonal fluctuation requires specialist care, but certain signs warrant a referral. Primary care doctors often suggest seeing an endocrinologist if:
- You have persistent symptoms like unexplained fatigue, weight changes, or mood swings.
- Blood tests show abnormal hormone levels, such as elevated TSH for thyroid issues.
- You’re managing a chronic condition like diabetes but need advanced control.
- Family history includes endocrine diseases, prompting screening for conditions like autoimmune thyroiditis.
For children, growth delays or early puberty signs are red flags. In adults, symptoms like erectile dysfunction or irregular menstrual cycles may indicate underlying issues. Early intervention can prevent complications, emphasizing the importance of timely consultations.
Education and Training of Endocrinologists
Becoming an endocrinologist requires extensive education:
- Undergraduate Degree: Typically in biology or pre-med, lasting 4 years.
- Medical School: 4 years of MD or DO training.
- Residency: 3 years in internal medicine or pediatrics.
- Fellowship: 2-3 years specializing in endocrinology, including research and clinical rotations.
Board certification from organizations like the American Board of Internal Medicine ensures expertise. Many endocrinologists pursue subspecialties, such as diabetology or neuroendocrinology, and stay updated through continuing medical education on topics like emerging GLP-1 agonists for weight loss.
What to Expect During a Visit to an Endocrinologist
Your first appointment might last 30-60 minutes. Prepare by bringing medical history, current medications, and symptom logs. The endocrinologist will:
- Review your history and perform a physical exam, checking for goiters or swollen lymph nodes.
- Order tests like HbA1c for diabetes or DEXA scans for bone density.
- Discuss lifestyle factors, such as diet and exercise, which play a key role in hormonal health.
Follow-up visits monitor progress, adjusting treatments as needed. Patient education is central, empowering you to manage conditions effectively.
The Importance of Endocrinologists in Modern Healthcare
In an era of rising chronic diseases, endocrinologists are pivotal. Diabetes alone affects over 400 million people worldwide, contributing to healthcare costs exceeding $700 billion annually. Their work extends to public health initiatives, like obesity prevention programs, and research into innovative therapies, such as continuous glucose monitors or gene editing for endocrine cancers.
Moreover, with aging populations, issues like osteoporosis and hormonal cancers are surging. Endocrinologists collaborate in multidisciplinary teams, improving outcomes in fields like oncology and cardiology. Their role in transgender healthcare, providing safe hormone therapy, underscores their adaptability to societal needs.
Lifestyle Tips for Hormonal Health
While not a substitute for professional care, maintaining hormonal balance involves:
- A balanced diet rich in iodine for thyroid health and fiber for blood sugar control.
- Regular exercise to combat insulin resistance.
- Stress management techniques like meditation, as chronic stress elevates cortisol.
- Adequate sleep, which regulates hormones like melatonin and growth hormone.
Consult an endocrinologist before starting supplements, as excesses can disrupt balance.
Conclusion: Empowering Your Health Journey
Endocrinologists are unsung heroes in the fight against hormonal disorders, offering expertise that enhances quality of life. Whether dealing with diabetes management, thyroid treatment, or fertility challenges, their specialized knowledge is invaluable. If you’re experiencing symptoms or have risk factors, don’t hesitate to seek a referral. By understanding “what an endocrinologist does” and recognizing when to consult one, you take proactive steps toward better health.
This guide aims to inform and educate, but remember, it’s not medical advice. Always consult healthcare professionals for personalized guidance. With ongoing advancements in endocrinology, the future holds promise for even more effective treatments.