How Do You Get a Yeast Infection? Causes, Risk Factors, and Prevention
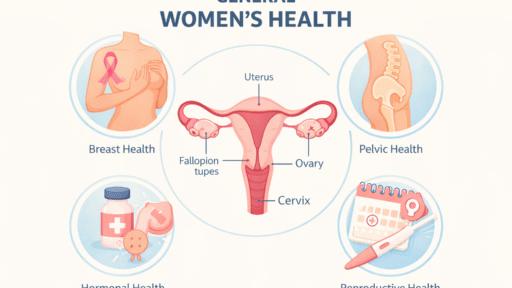
Yeast infections are one of the most common fungal infections worldwide, affecting millions of people each year. While they are often associated with women’s health, yeast infections can affect anyone, regardless of age or gender. Understanding how you get a yeast infection, what causes it, and how to prevent it is essential for maintaining overall health and avoiding recurring infections.
This article explains yeast infections in a clear, medically accurate, and AdSense-compliant way, while targeting high-CPC health keywords such as yeast infection causes, symptoms, treatment, prevention, and medical advice.
What Is a Yeast Infection?
A yeast infection, medically known as candidiasis, is caused by an overgrowth of a fungus called Candida. Candida normally lives on the skin and inside the body (mouth, throat, gut, and genital area) without causing harm. Problems occur when the balance between yeast and healthy bacteria is disrupted.
When yeast grows uncontrollably, it can lead to uncomfortable symptoms such as itching, irritation, redness, and discharge, depending on the area affected.
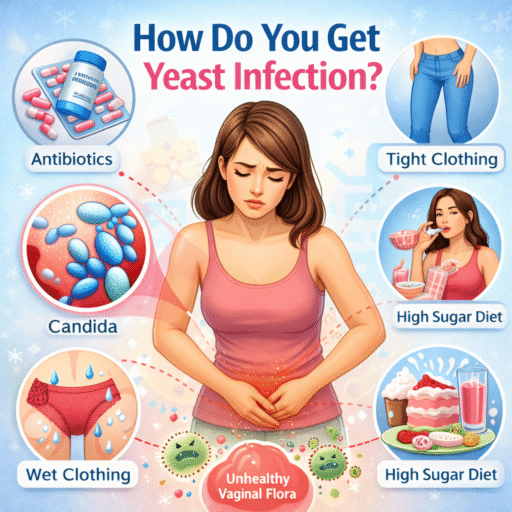
How Do You Get a Yeast Infection?
Yeast infections develop when conditions allow Candida to multiply beyond normal levels. Below are the most common causes and contributing factors.
1. Weakened Immune System
A healthy immune system keeps yeast under control. When immunity is weakened, yeast can grow more easily.
Common reasons for a weakened immune system include:
-
Chronic stress
-
Poor nutrition
-
Lack of sleep
-
Long-term illness
-
Certain medical treatments
People with compromised immunity are more vulnerable to frequent or severe yeast infections.
2. Antibiotic Use
Antibiotics are designed to kill harmful bacteria, but they often eliminate beneficial bacteria as well. These good bacteria normally help control yeast growth.
When antibiotics reduce healthy bacteria:
-
Yeast faces less competition
-
Candida can multiply rapidly
-
Infection risk increases
This is one of the most common triggers of yeast infections, especially after prolonged antibiotic use.
3. Hormonal Changes
Hormonal fluctuations can alter the body’s natural balance, making it easier for yeast to grow.
Hormonal changes may occur due to:
-
Pregnancy
-
Menstrual cycle variations
-
Hormonal medications
-
Certain contraceptives
These changes can affect moisture levels and natural defenses, increasing susceptibility to yeast infections.
4. High Blood Sugar Levels
Elevated blood sugar creates an environment where yeast thrives.
This is especially important for individuals with:
-
Diabetes
-
Insulin resistance
-
Poor blood sugar control
Excess sugar provides nourishment for yeast, allowing it to multiply more quickly.
5. Excess Moisture and Poor Air Circulation
Yeast thrives in warm, moist environments. Wearing tight or non-breathable clothing can trap moisture and heat against the skin.
Common contributors include:
-
Tight underwear
-
Synthetic fabrics
-
Staying in wet clothing for long periods
-
Excessive sweating
These conditions can encourage yeast overgrowth, particularly in skin folds.
6. Poor Hygiene Practices
Both poor hygiene and excessive cleansing can increase infection risk.
Examples include:
-
Not keeping skin clean and dry
-
Using heavily scented soaps or sprays
-
Frequent douching or harsh cleansers
These practices can disrupt the natural balance of microorganisms and irritate sensitive skin.
7. Diet High in Sugar and Refined Carbohydrates
Candida feeds on sugar. Diets high in:
-
Sugary foods
-
Refined carbohydrates
-
Processed snacks
may promote yeast overgrowth, especially when combined with other risk factors.
Common Symptoms of a Yeast Infection
Symptoms vary depending on the location of the infection but may include:
-
Itching or irritation
-
Redness or swelling
-
Thick discharge or skin changes
-
Burning sensation during daily activities
-
Discomfort or soreness
If symptoms persist or worsen, medical evaluation is recommended.
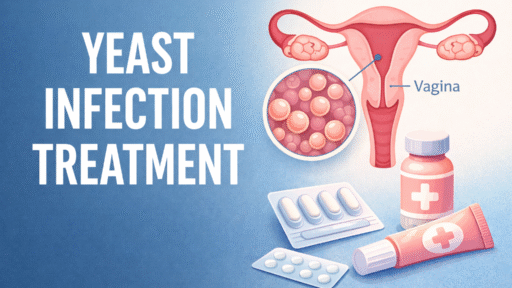
How Are Yeast Infections Diagnosed?
A healthcare professional may diagnose a yeast infection through:
-
Medical history review
-
Physical examination
-
Laboratory testing if necessary
Accurate diagnosis is important, as symptoms may resemble other conditions requiring different treatments.
How to Prevent Yeast Infections
Preventive strategies focus on maintaining balance and reducing risk factors.
Key Prevention Tips:
-
Wear breathable, loose-fitting clothing
-
Maintain good hygiene without over-cleansing
-
Keep skin clean and dry
-
Manage blood sugar levels
-
Eat a balanced, nutrient-rich diet
-
Use antibiotics only when prescribed
-
Manage stress and get adequate sleep
These steps can significantly reduce the likelihood of recurring infections.
When to See a Doctor
You should consult a healthcare provider if:
-
Symptoms are severe or recurring
-
You are unsure of the diagnosis
-
Home care does not improve symptoms
-
You have underlying health conditions
Professional guidance ensures safe and effective treatment.
Frequently Asked Questions (FAQs)
Are yeast infections contagious?
Yeast infections are generally not considered contagious, but shared environments and certain conditions may increase risk.
Can men get yeast infections?
Yes. Yeast infections can affect anyone, including men.
Can yeast infections go away on their own?
Mild cases may improve, but untreated infections can worsen or recur.
Final Thoughts
Understanding how you get a yeast infection is the first step toward prevention and long-term health. Most yeast infections result from an imbalance in the body’s natural environment, often triggered by lifestyle factors, medications, or health conditions. With proper care, hygiene, and medical guidance, yeast infections are manageable and often preventable.
Disclaimer: This article is for informational purposes only and does not replace professional medical advice. Always consult a qualified healthcare provider for diagnosis and treatment.
Yeast infections are one of the most common fungal infections worldwide, affecting millions of people each year. While they are often associated with women’s health, yeast infections can affect anyone, regardless of age or gender. Understanding how you get a yeast infection, what causes it, and how to prevent it is essential for maintaining overall health and avoiding recurring infections.
This article explains yeast infections in a clear, medically accurate, and AdSense-compliant way, while targeting high-CPC health keywords such as yeast infection causes, symptoms, treatment, prevention, and medical advice.
What Is a Yeast Infection?
A yeast infection, medically known as candidiasis, is caused by an overgrowth of a fungus called Candida. Candida normally lives on the skin and inside the body (mouth, throat, gut, and genital area) without causing harm. Problems occur when the balance between yeast and healthy bacteria is disrupted.
When yeast grows uncontrollably, it can lead to uncomfortable symptoms such as itching, irritation, redness, and discharge, depending on the area affected.
How Do You Get a Yeast Infection?
Yeast infections develop when conditions allow Candida to multiply beyond normal levels. Below are the most common causes and contributing factors.
1. Weakened Immune System
A healthy immune system keeps yeast under control. When immunity is weakened, yeast can grow more easily.
Common reasons for a weakened immune system include:
-
Chronic stress
-
Poor nutrition
-
Lack of sleep
-
Long-term illness
-
Certain medical treatments
People with compromised immunity are more vulnerable to frequent or severe yeast infections.
2. Antibiotic Use
Antibiotics are designed to kill harmful bacteria, but they often eliminate beneficial bacteria as well. These good bacteria normally help control yeast growth.
When antibiotics reduce healthy bacteria:
-
Yeast faces less competition
-
Candida can multiply rapidly
-
Infection risk increases
This is one of the most common triggers of yeast infections, especially after prolonged antibiotic use.
3. Hormonal Changes
Hormonal fluctuations can alter the body’s natural balance, making it easier for yeast to grow.
Hormonal changes may occur due to:
-
Pregnancy
-
Menstrual cycle variations
-
Hormonal medications
-
Certain contraceptives
These changes can affect moisture levels and natural defenses, increasing susceptibility to yeast infections.
4. High Blood Sugar Levels
Elevated blood sugar creates an environment where yeast thrives.
This is especially important for individuals with:
-
Diabetes
-
Insulin resistance
-
Poor blood sugar control
Excess sugar provides nourishment for yeast, allowing it to multiply more quickly.
5. Excess Moisture and Poor Air Circulation
Yeast thrives in warm, moist environments. Wearing tight or non-breathable clothing can trap moisture and heat against the skin.
Common contributors include:
-
Tight underwear
-
Synthetic fabrics
-
Staying in wet clothing for long periods
-
Excessive sweating
These conditions can encourage yeast overgrowth, particularly in skin folds.
6. Poor Hygiene Practices
Both poor hygiene and excessive cleansing can increase infection risk.
Examples include:
-
Not keeping skin clean and dry
-
Using heavily scented soaps or sprays
-
Frequent douching or harsh cleansers
These practices can disrupt the natural balance of microorganisms and irritate sensitive skin.
7. Diet High in Sugar and Refined Carbohydrates
Candida feeds on sugar. Diets high in:
-
Sugary foods
-
Refined carbohydrates
-
Processed snacks
may promote yeast overgrowth, especially when combined with other risk factors.
Common Symptoms of a Yeast Infection
Symptoms vary depending on the location of the infection but may include:
-
Itching or irritation
-
Redness or swelling
-
Thick discharge or skin changes
-
Burning sensation during daily activities
-
Discomfort or soreness
If symptoms persist or worsen, medical evaluation is recommended.
How Are Yeast Infections Diagnosed?
A healthcare professional may diagnose a yeast infection through:
-
Medical history review
-
Physical examination
-
Laboratory testing if necessary
Accurate diagnosis is important, as symptoms may resemble other conditions requiring different treatments.
How to Prevent Yeast Infections
Preventive strategies focus on maintaining balance and reducing risk factors.
Key Prevention Tips:
-
Wear breathable, loose-fitting clothing
-
Maintain good hygiene without over-cleansing
-
Keep skin clean and dry
-
Manage blood sugar levels
-
Eat a balanced, nutrient-rich diet
-
Use antibiotics only when prescribed
-
Manage stress and get adequate sleep
These steps can significantly reduce the likelihood of recurring infections.
When to See a Doctor
You should consult a healthcare provider if:
-
Symptoms are severe or recurring
-
You are unsure of the diagnosis
-
Home care does not improve symptoms
-
You have underlying health conditions
Professional guidance ensures safe and effective treatment.
Frequently Asked Questions (FAQs)
Are yeast infections contagious?
Yeast infections are generally not considered contagious, but shared environments and certain conditions may increase risk.
Can men get yeast infections?
Yes. Yeast infections can affect anyone, including men.
Can yeast infections go away on their own?
Mild cases may improve, but untreated infections can worsen or recur.
Final Thoughts
Understanding how you get a yeast infection is the first step toward prevention and long-term health. Most yeast infections result from an imbalance in the body’s natural environment, often triggered by lifestyle factors, medications, or health conditions. With proper care, hygiene, and medical guidance, yeast infections are manageable and often preventable.
Disclaimer: This article is for informational purposes only and does not replace professional medical advice. Always consult a qualified healthcare provider for diagnosis and treatment.